Improving Access to Oncology Nutrition Services
Author(s):
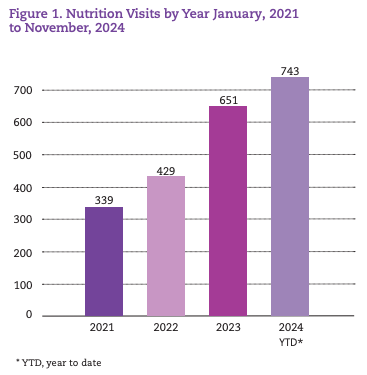
Access to nutrition services for patients with cancer who are at risk for treatment- and disease-related issues such as malnutrition, dehydration, nausea, and diarrhea is a key component of the care pathway. Even with specialists available, the biggest challenge can be to successfully connect patients to these services. This connection point is improved by reducing barriers and optimizing processes—and Cape Cod Healthcare in Hyannis, Massachusetts, is achieving success with both of these tasks. For example, use of various strategies and collaborative problem-solving in Cape Cod Healthcare’s nutrition services program led to a greater than 50% growth in volume (223 patients) from 2022–2023; further, 52 unique patients (16%) were served, and more patients were connected to needed nutrition services (Figure 1).
Identifying Areas for Improvement
In 2020, 4 patients were seen per day on average in our nutrition program, although the goal was an average of 6 patients. As a result, fewer hours were dedicated to the program to match the seemingly low demand. Despite daily volumes being below target, the staff had a strong sense that there was an unmet need. Creating systems to connect patients to nutrition services and, in turn, demonstrating an increased patient demand became the operational focus. The staff observed several areas that could be improved.
- Staff in the medical and radiation oncology units used an evidencebased and electronic health record (EHR)–integrated malnutrition screening tool in their patient rooming process. However, the workflow was not optimized to ensure that dietitian appointments were made for screened patients at high risk.
- No consistent pathway was available to connect patients with head and neck and certain gastrointestinal (GI) cancers with dietitians early in their care; in addition, a standard follow-up frequency was also lacking.
- The ordering process and associated follow-up for enteral feeding tube placement and support through outside durable medical equipment (DME) vendors were unclear and inefficient.
- The Rehabilitation Department sought ways to hasten identification of oncology patients needing speech pathology support and to help reduce barriers for patients to keep appointments. These were many of the same patients who needed nutrition services.

Implementing Solutions
Screening Process
For patients who were at nutritional high risk according to a screening, we created a build in the EHR as part of our rooming process. This build triggers a best-practice alert for the nurse or medical assistant to send a message to the scheduling team via the Epic In Basket (Epic Systems, Inc) to schedule an appointment with the dietitian. This process ensures direct communication for scheduling a nutrition visit based on patient screening results. The workflow is now being enhanced to allow referrals to be routed to a scheduler work queue in Epic rather than to an In-Basket message; in addition, it would allow patients to schedule their own appointments in MyChart (Epic Systems, Inc).
Pathway for Head and Neck and GI Cancers
A team convened to review and improve the process for connecting high-risk patients to nutrition services (eg, tube feeding referrals, support). From this work, the following improvements were made:
- Referrals are consistently placed with the dietitian directly after the radiation oncologist’s initial consultation; these patients are now seen weekly in follow-up by the dietitian for 12 weeks.
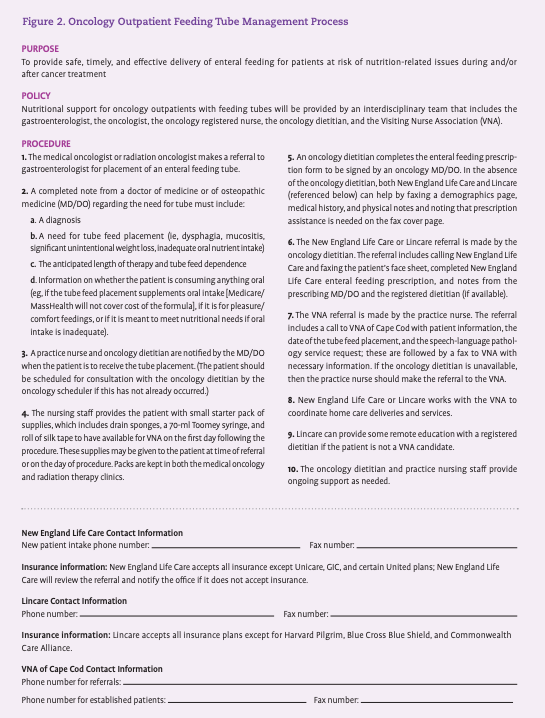
- A process was developed (Figure 2) to define roles and responsibilities for feeding tube placement after a physician referral is made. In addition, nurses developed feeding tube starter kits containing needed supplies and printed instructions for patients.
- To facilitate efficiency in ordering feeding tube formula with outside vendors, the Epic team developed a workflow for the dietitian to place DME orders that leverages a SmartPhrase with SmartLists in the order comments. The SmartPhrases and SmartLists were modeled after the paper packets that had previously been faxed. The order containing populated SmartPhrases/SmartLists and all the needed medical record information then gets routed from Epic directly to the DME vendor.
“We are able to identify and address the patient’s needs effectively and efficiently given our access to the care team, which can often prevent hospitalization.” SPEECH-LANGUAGE PATHOLOGIST MELANIE REYNOLDS
Collaboration With Rehabilitation
Excellent speech pathology services are available for patients with cancer at Cape Cod Hospital, but these services are available in a different location from the cancer center. Recognizing that multiple appointments in various settings can be a barrier for patients, the cancer center created a speech and nutrition clinic that provides 1 multidisciplinary initial assessment with both a dietitian and a speech-language pathologist. These assessments are offered twice monthly. Since inception in December 2022, 35 patients have had these assessments in this clinic.
The combined speech and nutrition evaluation results in a comprehensive evaluation and education experience for each patient newly diagnosed with head and neck cancer. During this 90-minute session, the speech-language pathologist gathers information regarding the patient’s baseline level of swallow functioning including the history of previous swallow assessments, the current diet consistency, and additional medical diagnoses that may impact swallow function. Any upcoming or past surgeries related to the patient’s head and neck cancer are reviewed. At the conclusion of this initial consultation, the speech-language pathologist makes recommendations regarding the most appropriate diet level, compensatory swallowing techniques, and prophylactic exercises to preserve strength and range of motion of the swallowing musculature. Potential acute and chronic effects of radiation on the swallow mechanism and the expected impact of radiation treatment (eg, dry mouth, inflamed oral mucosa, altered taste) on the patient’s oral, pharyngeal, and laryngeal mucosa are discussed. Techniques to manage these potential adverse effects are discussed to maximize the patient’s ability to maintain oral intake throughout and after radiotherapy.
“Undergoing radiation treatment is a time consuming and overwhelming process for our patients,” shared speech-language pathologist Melanie Reynolds. “The ability to address their dysphagia rehabilitation needs at the same location they received their radiation treatment is not only more convenient for the patient, but it allows for better communication between the speech-language pathologist and the medical team, resulting in more effective treatment with better outcomes.”
The speech-language pathologist also now holds a follow-up clinic in radiation oncology once weekly to ensure needed follow-up after the clinic visit. Whenever possible, patients are scheduled directly after or before their radiation treatment.
“We initiated this program 11 months ago, and, in that time, we have seen these patients for 119 visits and have experienced an 18% no-show/cancellation rate,” said Sarah Lessard-Reiss, the manager of outpatient rehabilitation services. “During the year prior, when the patients were scheduled in a separate location and did not have the convenience of being seen in radiation oncology, we recorded a 25% no-show/cancellation rate, so it has been great to see this improvement in patients attending their appointments.” Reynolds continued, “We are able to identify and address the patient’s needs effectively and efficiently given our access to the care team, which can often prevent hospitalization.”
The collaboration with the speech-language pathologist in a joint initial assessment allows the dietitian to have more in-depth knowledge about the patient’s current swallowing ability so that nutrition recommendations can be tailored appropriately. Many patients have baseline chewing and/or swallowing challenges due to surgeries, biopsies, pain, or the actual tumor placement.
Once the patient’s treatment begins, a collaboration between the registered dietitian and the speech-language pathologist and knowledge of recommendations based on results of a current modified barium swallow test allow for more detailed nutrition recommendations to be provided. Both the speech-language pathologist and the registered dietitian follow patients weekly during treatment and 3 to 6 weeks or longer after completion of treatment. This weekly follow-up by the registered dietitian allows for closer observation of any changes in the intake of fluid and solids by mouth and evaluation of whether nutritional needs are being met. Weekly follow-up also allows for modifications to the nutrition supplement plan and avoidance of the need for percutaneous endoscopic gastrostomy (PEG) tube placement. In some cases, use of a PEG tube may be needed if other strategies are deemed unsuccessful to lower the risk of protein-calorie malnutrition.

Today, there is ongoing dialogue and collaboration between the speech-language pathologist and the registered dietitian. The registered dietitian can benefit from information about what the patient can do functionally. This is crucial for patients who may have had a PEG tube placed and who are working toward weaning off feeds or just advancing the texture of their diet. Patients greatly appreciate this collaborative support during such a challenging time.
Building on Success and Integrating Nursing Practice
Oncology nurses are typically the first to hear from patients who are struggling with treatment-related adverse events and cancer-related symptoms. Cape Cod Healthcare wanted to support a collaborative effort between nursing staff and dietitians to identify and support any nutritional needs that may negatively impact a patient’s well-being and tolerance of cancer treatment.

Toward this end, Cape Cod Healthcare has built on the success noted with nutrition and speech-language therapy and engaged with oncology nurses and nurse practitioners to review cases of patients admitted to the emergency department (ED). The cancer program worked with Epic to identify patients with cancer who reported to the ED for certain diagnoses within 30 days of receiving chemotherapy as part of its work on OP-35. (This publicly reported quality measure from the Centers for Medicare & Medicaid Services aims to decrease ED visits and resulting inpatient stays by encouraging cancer programs to develop proactive approaches to manage symptoms and adverse events.) The measure includes diagnoses of nausea, vomiting, diarrhea, dehydration, neutropenia, anemia, pain, pneumonia, fever, or sepsis.
Cape Cod Healthcare clinicians surmised that patients reporting nausea, vomiting, diarrhea, and dehydration could all be positively impacted by appropriate and proactive use of the nutrition services program. In addition, enhanced nursing triage assessment, acute visits with nurse practitioners and/or dietitians, and same-day hydration and electrolyte replenishment were also identified as important ways to improve patient symptom management and quality of life (QOL) and to keep patients out of the ED.
To obtain a baseline data measurement, for 4 months, the nursing team tracked patients who reported to the ED with OP-35 diagnoses; they found that 30% to 50% of these patients went to the ED for nausea, vomiting, diarrhea, and/or dehydration. The nursing team also included patients who sought care for constipation and abdominal pain, as pain is an OP-35 diagnosis that often resolved once the constipation was addressed. Cape Cod Healthcare found that of those 30% to 50% of patients, 65% to 100% of these individuals were not managed by a dietitian. Furthermore, over half of the patients who had dietitian involvement only had an initial visit but no recent follow-up prior to their ED visit. Based on this baseline data analysis, Cape Cod Healthcare believed that quality improvements could be made with earlier and improved assessments and interventions.
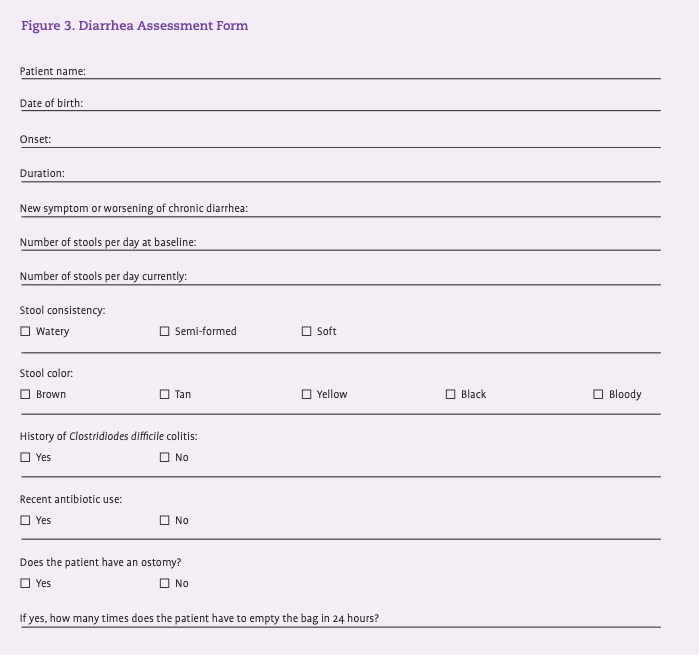
One quality improvement implemented is a partnership between nurses and nurse practitioners to develop standardized assessment forms for triage of various symptoms (eg, diarrhea) (Figure 3). These forms are then turned into a SmartPhrase in Epic that can be entered as a telephone encounter and forwarded to the nurse practitioner’s In Basket. The nurse and nurse practitioner work together with the patient to determine whether an acute visit with the nurse practitioner and hydration or medication management is needed. This enhanced triage assessment allows the nurse to decide whether a patient should work with the dietitian to improve the QOL at home and their compliance with the continued chemotherapy and/or radiotherapy regimen.
Cape Cod Healthcare’s work toward improving patient access to nutrition services dovetailed perfectly with its work to prevent ED admissions; in addition, it created collaboration opportunities for many team members. Cape Cod Healthcare plans to build on this success to identify more ways to best connect patients with needed support services and to help improve their QOL.
Katie Michaud, MPA, FACHE, is executive director of oncology services; Shelley West, MSN, RN, OCN, MBA, is director of oncology nursing and infusion services; and Abigail Usen Berner, MS, RD, LDN, is an oncology dietitian at Cape Cod Healthcare in Hyannis, Massachusetts.
Our Oncology Nutrition Program At a Glance
Established in 2016, the Oncology Nutrition Program at Cape Cod Healthcare provides free, personalized, and evidence-based medical nutrition therapy for patients undergoing treatment for cancer. Abigail Berner, MS, RD, LDN, a registered dietitian, works with staff and physicians to provide recommendations that are based on current research and tailored to a patient’s specific cancer diagnosis. The program provides patients with nutritional goals for treatment to maximize the nutritional quality of the diet and to navigate the following:
- Nutrition-related adverse effects during and after treatment
- Weight loss and weight gain management
- The use of multivitamins, minerals, and other natural/ herbal products
- Management of specialized diets and tube feeding regimens • Nutritional goals for cancer survivors.