Bridging Oncology and Dermatology: Integrating Dermatologic Toxicity Management Into Routine Cancer Care
Author(s):
An estimated 50% of patients with cancer experience disruptions in treatment due to dermatologic toxicity.
Anticancer treatment strategies have grown in number and complexity in recent decades, as have the toxicity profiles associated with these therapeutic agents. The increasing use of novel cancer therapies—including molecular targeted therapies, immunotherapies, hormonal therapies, and combinations of these—has introduced new dermatologic toxicities that differ significantly from those observed with traditional cytotoxic chemotherapy. Although these treatments have revolutionized cancer care, they frequently result in dermatologic complications such as hand-foot skin reaction, acneiform rash/ papulopustular eruption, xerosis, pruritus, mucositis, alopecia, nail changes, and more. These conditions not only cause physical discomfort but also contribute to emotional distress, financial burdens, and psychosocial challenges for patients. More severe dermatologic adverse events (AEs) can necessitate pauses in potentially lifesaving cancer treatment.
Recent efforts have been made to systematically approach the prevention, diagnosis, and management of these toxicities by bridging the expertise of dermatologists and oncologists. The first clinic dedicated to providing dermatologic supportive care to patients with cancer was established at Northwestern University in 2006.1 Since then, the subspecialized field of supportive oncodermatology has emerged to meet the needs of patients undergoing treatment for cancer as well as the expanding survivor population.
Given the growing number of cancer survivors and increased incidence and complexity of dermatologic AEs, there is an urgent need for effective collaboration between oncology and dermatology professionals. Unfortunately, access to dermatologic expertise remains limited, particularly in community oncology settings. Currently, only a few specialized oncodermatology services exist in major academic cancer centers, leaving many community practitioners without timely dermatologic support. Additionally, the rapid expansion of novel oncology therapeutics presents a learning curve for all clinicians, including dermatologists practicing in the community, as new and unique toxicity profiles continue to emerge.
An Unmet Need
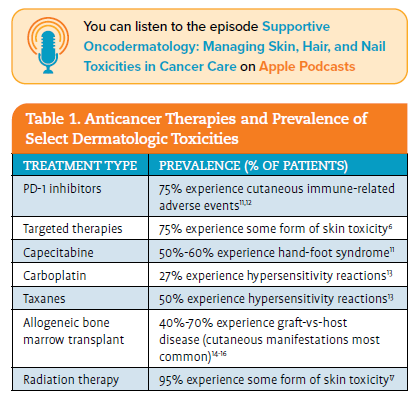
Although diagnosis and symptom severity will vary, most patients receiving cancer therapy will experience a dermatologic AE at some point during their treatment course (see Table 1). Timely evaluation by an experienced dermatologist can mitigate (or even prevent) many cutaneous toxicities, allowing patients to adhere to treatment plans where they may have otherwise interrupted therapy. Maintaining dose intensity is important to optimize outcomes for patients receiving chemotherapy and targeted treatment.3-5 Evidence demon strates that patients with a cutaneous toxicity who see a dermatologist are less likely to experience treatment interruption.6-8 Given that an estimated 50% of patients with cancer experience disruptions in treatment due to dermatologic toxicity,9 supportive oncodermatology services are necessary for maximizing clinical outcomes and improving quality of life for patients receiving treatment for cancer. With an estimated 2,001,140 new cases of cancer diagnosed in the US in 2024,10 the need for accessible supportive oncodermatology services cannot be overstated.

“A Practice Within a Practice”
The opportunity for prompt evaluation by an oncodermatology specialist is necessary for several reasons. Urgent oncodermatology consultation can:
- Confirm the diagnosis of cutaneous toxicity, including grading severity (which informs real-time decision-making for cancer treatment).
- Assess whether the condition is likely related to cancer treatment and, if it is, guide the decision to continue, hold, or discontinue cancer therapy.
- Enable patients to avoid reflex steroid treatment, which can mask symptom manifestation and thus confound dermatologic diagnosis and severity assessment.
- Provide nuanced, individualized recommendations to patients experiencing dermatologic AEs.
The best possible scenario to facilitate timely accessibility of dermatologic expertise is the integration of specialized oncodermatology within the same cancer practice where the patient is receiving cancer treatment. Embedding oncodermatology into routine cancer care can prevent or promptly address dermatology AEs. The oncodermatology clinic would need to be supplied with the appropriate equipment for biopsies and bedside diagnostics.
If integration into an individual cancer practice itself is not possible, on-site access within the same cancer center or physical location can also be helpful. Colocation helps to coordinate care between the oncology and dermatology departments and limits logistical hurdles for patients and caregivers. It is useful to clarify which dermatologists (or dermatology advanced practice providers) are the preferred contacts for supportive oncodermatology and to make their contact information available to the oncologists at that institution. A successful example of this is a cancer center that implemented same-day consultation practices, reserving several daily appointments in the dermatology clinic to address urgent oncology treatment–related issues. As explained in focus groups conducted by the Association of Cancer Care Centers (ACCC), the opportunity for urgent-access appointments allows the cancer team to have oncodermatologic expertise to inform cancer treatment decisions. Another institution has a practice of coscheduling follow-up appointments with oncology and dermatology on the same day, alleviating financial and travel burdens on patients and care- givers. Lastly, one focus group participant shared their success with implementing intra-institution texting between dermatology advanced practice providers and oncologists so that urgent cases could be addressed on a real-time basis.
Off-Site Referrals
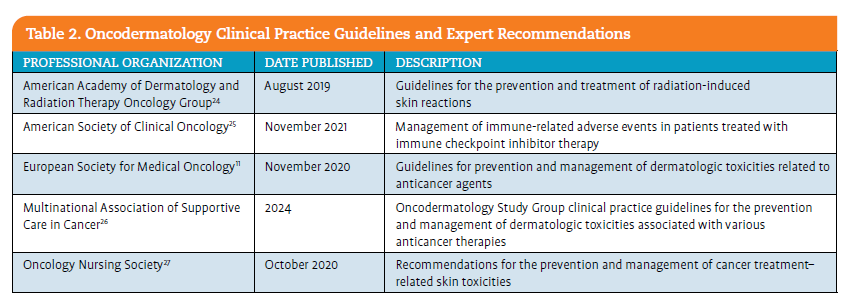
When practice integration or colocation are not feasible, referring patients to oncodermatology specialists remains important for managing patients with dermatologic AEs or monitoring those receiving high-risk cancer therapies. Community dermatologists with experience in oncology-related AEs can also play a key role in patient care. Numerous educational resources are available to help general dermatologists expand their knowledge of treatment-related AEs associated with novel cancer therapies (see Table 2). Ensuring timely access to dermatologic expertise is essential for supporting oncology treatment decisions. Utilizing digital technology to standardize workflows, clinical photography, and docu- mentation can help streamline this process and enhance collabo- ration between dermatology and oncology teams.
One approach to expanding oncodermatology access in community or geographically remote settings is the use of eConsult and teledermatology services. For example, one site has piloted an eConsult initiative across its medical system, in which oncology teams capture and upload clinical images into the electronic health record (EHR). Dermatologists then promptly review these images, provide recommendations, and determine whether an in-person visit is necessary for further evaluation or biopsy. This process ensures a rapid turnaround, often within 48 hours, allowing those with dermatologic expertise to guide cancer care on a case-by-case basis. Teledermatology was also identified as a potential solution for community cancer centers where on-site dermatologic expertise is unavailable. Through virtual consultations, oncodermatologists can assess toxicities, offer management recommendations, and guide oncology teams on next steps. These strategies enhance accessibility and expedite care, reducing delays in addressing dermatologic complications of cancer therapies.
A major challenge reported in focus groups concerning off-site oncodermatology referrals is the inconsistency in documentation and referral quality. Oncology providers sometimes struggle to communicate detailed and accurate descriptions of dermatologic adverse events, making it difficult to ensure appropriate triage and diagnosis. Compounding this issue is the fact that patients may not always fully report symptoms, and a full dermatologic exam is often impractical outside a clinic setting. Without standardized documentation, clinical photographs, and clinical context, deter- mining the urgency of a referral can be challenging. Implementing structured protocols, such as standardized photography guidelines and clear triage criteria, could improve referral accuracy. For instance, one site has introduced a dedicated oncodermatology referral order set within the EHR, ensuring that oncology patients
This approach fosters patient engagement, reduces anxiety, and promotes adherence to recommended prophylactic regimens. By setting realistic expectations and establishing lines of communication early, cancer care teams can empower patients to recognize and address initial signs of cutaneous toxicity. Patients often hesitate to disclose emerging signs of dermatologic toxicity for fear of the need to interrupt treatment. When patients are advised that early recognition can reduce the severity of many toxicities and therefore prevent treatment interruptions, they are much more comfortable communicating with the care team about AEs involving the skin, hair, or nails.
Proper and consistent skin care practices at home can significantly reduce the severity of many dermatologic AEs. Patients should be advised to use gentle, fragrance-free cleansers and moisturizers to maintain skin hydration and barrier function. Sun protection is also critical, as photosensitivity is a common adverse event associated with many oncologic therapies. Certain treat- ment-specific interventions (eg, prophylactic application of topical antibiotics) may be beneficial depending on the treatment regimen. A meta-analysis evaluated the ability of prophylactic antibiotics to reduce the risk of acneiform rash associated with anti-EGFR agents. The study data showed that moderate to severe toxicities (grades 2-4) were reduced by nearly two-thirds.18 Other evidence- based strategies are emerging in the literature, such as antihistamine
prophylaxis for rash associated with the PI3Kα inhibitor alpelisib.19 More recently, data from the first interim analysis of the phase 2 COCOON study (NCT06120140) demonstrate that a proactive dermatologic regimen along with amivantamab-vmjw and lazertinib can significantly reduce the frequency of both skin- and nail-related adverse events associated with EGFR inhibitors.20 Oncology providers can find a list of useful skin care recommendations for all patients at risk for dermatologic toxicity in the ACCC publication “Preventing and Managing Common Dermatologic Toxicities: A Guide for Clinicians.”
For patients receiving high-risk therapies, automatic referral to oncodermatology can be a valuable component of prophylactic management. EGFR inhibitors, for instance, are well known for their high incidence of dermatologic toxicities, including acneiform rash, xerosis, and pruritus. Early dermatologic consultation can provide tailored recommendations for prophylaxis, such as preemptive topical or systemic therapies, to minimize complications and improve adherence to cancer treatment. In a study of 95 patients receiving targeted therapy affecting the cell growth pathway, 48 followed a proactive skin care regimen, and 47 received reactive treatment after symptoms developed. The incidence of severe skin toxicities in the proactive group was reduced by 50% compared with the reactive group, underscoring the importance of early intervention. 21 Moreover, dermatology consultation prior to receiving cancer therapy has led to reduced interruption of oncology treatment.22
Although proactive management is essential, it is equally important to strike a balance between providing comprehensive anticipatory guidance and avoiding overwhelming patients who are already navigating complex treatment regimens. Clinicians should tailor their recommendations based on individual risk factors, treatment type, and patient preferences. Clear, concise education with actionable steps can help patients feel supported without becoming overburdened by excessive instructions. By integrating automatic referral (when appropriate) and prophylactic skin care into routine oncology care, clinicians can optimize treatment tolerance while improving patients’ overall experience.
Multidisciplinary Care Team Education
Educational resources must also incorporate diverse imaging to ensure that health care providers can accurately recognize dermatologic conditions in patients of all skin tones. Many dermatologic conditions present differently depending on skin pigmentation, and a lack of diverse reference materials can contribute to delayed or missed diagnoses, potentially worsening
patient outcomes. Addressing this gap in educational materials is a critical step toward promoting equitable care.
Institutional or virtual supportive care conferences, which may be purely oncodermatology or multidisciplinary depending on organizational needs, are a helpful forum for patient care discus- sion, as they greatly facilitate academic and clinical collaboration. One focus group participant communicated the value of holding regular multidisciplinary conferences involving dermatologists, medical oncologists, radiation oncologists, and other specialists as a way to discuss complex cases and share knowledge. At each conference, participants discuss 2 to 6 patient cases for 15 to 20 minutes each, as well as plans for management. Often, a review of the literature is presented, synthesized by a trainee and attending involved in each case. Another site implements weekly dermato- pathology case conferences, which include dermatologists and dermatopathologists, to solicit input and advice on various cases. Community cancer centers looking to implement these conferences may consider leveraging videoconferencing with local academic centers or dermatology colleagues interested in collaboration.
As one focus group participant noted, dermatology has many gray areas in terms of grading, treatment, and patient experience of each condition. Overly relying on an algorithmic approach to treatment can be risky, but more standardized protocols would be helpful. Oncology providers may find the ACCC publication “Preventing and Managing Common Dermatologic Toxicities: AGuide for Clinicians” to be a useful starting point to review common (and potentially severe) dermatologic toxicities as well as management strategies, including a clinical algorithm outlining when referral to oncodermatology is appropriate.
Ensuring that all cancer care team members have access to the education and resources they need to address dermatologic AEs will improve timely intervention, reduce patient distress, and opti- mize overall treatment outcomes. Clinician education can be facil- itated through professional societies, visiting lectures, grand rounds presentations by oncodermatologists, and CME conferences and workshops. Membership in the Oncodermatology Society or the MASCC Oncodermatology Study Group are excellent ways to learn more and contribute to the specialty. Clinical practice guidelines have been developed in recent years to standardize care for patients who experience dermatologic sequelae associated with anticancer therapies, reflecting the latest evidence and expert consensus regarding optimal clinical practice (see Table 2).

Conclusion
As the landscape of anticancer therapy continues to evolve, so does the spectrum of associated dermatologic toxicities. These adverse events are not merely cosmetic concerns but can significantly impact patient quality of life, treatment adherence, and overall clinical outcomes. The emerging field of supportive oncoderma- tology has made significant strides in addressing these challenges by integrating dermatologic expertise into oncology care. However, substantial gaps remain, particularly in community oncology settings where access to specialized dermatologic care is limited.
As demonstrated through successful institutional models and emerging best practices, integrating oncodermatology into routine cancer care is feasible, beneficial, and highly desired by patients with cancer. Standardized education, clinical guidelines, and structured workflows can further support this integration, ensuring that all patients—regardless of treatment setting—receive the dermatologic care necessary to optimize their oncologic outcomes.
Nicole A Colwell, MD is a senior editor/ medical writer at the Association of Cancer Care Centers (ACCC) in Rockville, Maryland.
This program is made possible with support by AstraZeneca and Johnson & Johnson.
References
- Lacouture ME, Basti S, Patel J, Benson A 3rd. The SERIES clinic: an interdisciplinary approach to the management of toxicities of EGFR inhibitors. J Support Oncol. 2006;4(5):236-238.
- Kaplan BW. The emerging role of supportive oncodermatology in multidisciplinary cancer care. Oncology Nurse Advisor. June 10, 2020. Accessed February 19, 2025. https://www.oncologynurseadvisor.com/ features/emerging-role-of-supportive-oncodermatology-in- multidisciplinary-cancer-care/2/
- Lyman GH. Impact of chemotherapy dose intensity on cancer patient outcomes. J Natl Compr Canc Netw. 2009;7(1):99-108. doi:10.6004/ jnccn.2009.0009
- Nielson CM, Bylsma LC, Fryzek JP, Saad HA, Crawford J. Relative dose intensity of chemotherapy and survival in patients with advanced stage solid tumor cancer: a systematic review and meta-analysis. Oncol- ogist. 2021;26(9):e1609-e1618. doi:10.1002/onco.13822
- Shirotake S, Yasumizu Y, Ito K, et al. Impact of second-line targeted therapy dose intensity on patients with metastatic renal cell carcinoma. Clin Genitourin Cancer. 2016;14(6):e575-e583. doi:10.1016/j. clgc.2016.03.014
- Long V, Choi ECE, Tan CL. Supportive oncodermatology—a narrative review of its utility and the way forward. Support Care Cancer. 2021;29(9):4931-4937. doi:10.1007/s00520-021-06124-w
- Jacoby TV, Shah N, Asdourian MS, et al. Dermatology evaluation for cutaneous immune-related adverse events is associated with improved survival in cancer patients treated with checkpoint inhibition. J Am Acad Dermatol. 2023;88(3):711-714. doi:10.1016/j.jaad.2022.09.012
- Yu Z, Dee EC, Bach DQ, Mostaghimi A, LeBoeuf NR. Evaluation of a comprehensive skin toxicity program for patients treated with epidermal growth factor receptor inhibitors at a cancer treatment center. JAMA Dermatol. 2020;156(10):1079-1085. doi:10.1001/jamadermatol.2020.1795
- Aizman L, Nelson K, Sparks AD, Friedman AJ. The influence of sup- portive oncodermatology interventions on patient quality of life: a cross-sec- tional survey. J Drugs Dermatol. 2020;19(5):477-482.
- Cancer statistics. National Cancer Institute. Updated May 9, 2024. Accessed February 19, 2025. cancer.gov/about-cancer/understanding/statistics
- Lacouture ME, Sibaud V, Gerber PA, et al; ESMO Guidelines Com- mittee. Prevention and management of dermatological toxicities related to anticancer agents: ESMO clinical practice guidelines. Ann Oncol. 2021;32(2):157-170. doi:10.1016/j.annonc.2020.11.005
- Robert C, Long GV, Brady B, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372(4):320-330. doi:10.1056/NEJMoa1412082
- Tsao LR, Young FD, Otani IM, Castells MC. Hypersensitivity reactions to platinum agents and taxanes. Clin Rev Allergy Immunol. 2022;62(3):432-448. doi:10.1007/s12016-021-08877-y
- Baumrin E, Loren AW, Falk SJ, Mays JW, Cowen EW. Chronic graft- versus-host disease: part I: epidemiology, pathogenesis, and clinical manifestations. J Am Acad Dermatol. 2024;90(1):1-16. doi:10.1016/j. jaad.2022.12.024
- Malard F, Holler E, Sandmaier BM, Huang H, Mohty M. Acute graft- versus-host disease. Nat Rev Dis Primers. 2023;9(1):27. doi:10.1038/ s41572-023-00438-1
- Bachier CR, Aggarwal SK, Hennegan K, et al. Epidemiology and treatment of chronic graft-versus-host disease post-allogeneic hematopoietic cell transplantation: a US claims analysis. Transplant Cell Ther. 2021;27(6):504.e1-504.e6. doi:10.1016/j.jtct.2020.12.027
- Wei J, Meng L, Hou X, et al. Radiation-induced skin reactions: mech- anism and treatment. Cancer Manag Res. 2018;11:167-177. doi:10.2147/ CMAR.S188655
- Petrelli F, Borgonovo K, Cabiddu M, et al. Antibiotic prophylaxis for skin toxicity induced by antiepidermal growth factor receptor agents: a systematic review and meta-analysis. Br J Dermatol. 2016;175(6):1166- 1174. doi:10.1111/bjd.14756
- Rugo HS, Lacouture ME, Goncalves MD, Masharani U, Aapro MS, O’Shaughnessy JA. A multidisciplinary approach to optimizing care of patients treated with alpelisib. Breast. 2022;61:156-167. doi:10.1016/j. breast.2021.12.016
- COCOON study meets primary end point demonstrating statistically significant and clinically meaningful reduction in dermatologic reactions with easy-to-use prophylactic regimen for patients with EGFR-mutated NSCLC. News release. Johnson & Johnson. January 14, 2025. Accessed
February 19, 2025. innovativemedicine.jnj.com/newsroom/cocoon-study-meets-primary-endpoint-demonstrating-statistically-signif-icant-and-clinically-meaningful-reduction-in-dermatologic-reac-tions-with-easy-to-use-prophylactic-regimen-for-patients-with-egfr-mu-tated-nsclc - Lacouture ME, et al. Skin toxicity evaluation protocol with panitumumab (STEPP), a phase II, open-label, randomized trial evaluating the impact of a preemptive skin treatment regimen on skin toxicities and quality of life in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28(8):1351-1357. doi:10.1200/JCO.2008.21.7828
- Chen ST, Molina GE, Lo JA, et al. Dermatology consultation reduces interruption of oncologic management among hospitalized patients with immune-related adverse events: a retrospective cohort study. J Am Acad Dermatol. 2020;82(4):994-996. doi:10.1016/j.jaad.2019.09.026
- Skripnik Lucas A, Ciccolini K. The role of oncodermatology in the care of patients receiving cancer therapy. Semin Oncol Nurs. 2017;33(4):393-401. doi:10.1016/j.soncn.2017.08.001
- Rosenthal A, Israilevich R, Moy R. Management of acute radiation dermatitis: a review of the literature and proposal for treatment algorithm. J Am Acad Dermatol. 2019;81(2):558-567. doi:10.1016/j.jaad.2019.02.047
- Schneider BJ, Naidoo J, Santomasso BD, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: ASCO guideline update. J Clin Oncol. 2021;39(36):4073- 4126. doi:10.1200/JCO.21.01440
- MASCC guidelines. Multinational Association of Supportive Care in Cancer. Accessed February 19, 2025. mascc.org/resources/mascc-guidelines/?refer=oncodermatology-study-group
- Williams LA, Ginex PK, Ebanks GL Jr, et al. ONS guidelines for cancer treatment–related skin toxicity. Oncol Nurs Forum. 2020;47(5):539-556. doi:10.1188/20.ONF.539-556. Accessed February 19, 2025. ons.org/publications-research/onf/47/5ons-guidelinestm-cancer-treatment-related-skin-toxicity















