Creating a Community-Wide Safety Net with Centralized Tracking and Management of Incidental Lung Nodules
Author(s):
Lung cancer is the second most common cancer among men and women and the leading cause of cancer-related death, accounting for 20% of all cancer deaths.1 Overall survival for lung cancer is still only 23%, largely because the majority of lung cancers are diagnosed at later stage.2 Although survival is much higher for early-stage disease, only 26% of patients with lung cancer are diagnosed at a localized stage.1 The National Lung Screening Trial demonstrated a 20% relative mortality benefit of lung cancer screening with yearly low-dose computed tomography.3 However, only 6% of people eligible for lung cancer in the US receive screening.4 Poor uptake is due to a combination of complex barriers at the patient, provider, and health system level. A promising avenue to diagnosis is identifi-cation and management of incidental lung nodules.
What Are Incidental Findings?
Incidental findings are unanticipated, potentially cancerous abnormalities that are found unintentionally on imaging scans and are unrelated to the condition that prompted the medical exam. Use of various imaging techniques is rising, leading to an increase in incidental findings. Approximately 15% to 30% of all diagnostic imaging and 20% to 40% of computed tomography (CT) exams contain at least 1 incidental finding.5 Most incidental findings have management and follow-up guidelines developed by relevant medical and surgical subspecialty societies.
In usual practice, a radiologist will read imaging and note any incidental findings in the imaging report. Only 40% of patients with incidental findings receive guideline-recommended follow up.6 Not all incidental findings noted by radiologists have recommendations included for follow up in the report. In a 2019 study of 1000 patients who received CT for traumatic injuries, radiologists gave recommendations for follow up 53.5% of the time, but only 13.9% of those patients ever received appropriate follow up.7 Incidental findings can easily be missed if buried within the body text of the imaging report and not included in the impression summary. In this same study, 47% of incidental findings were not mentioned in the impression but instead were in the body of the report.7 Furthermore, many incidental findings are not communicated to patients; 43% of patients in the study did not receive information about their incidental finding and their recommended follow up.7
Incidental Lung Nodules
Lung nodules, defined as spots or growths on the lung, are 1 of the most common incidental findings on imaging that includes the chest. Lung nodules are identified in approximately 1.6 million people per year in the US.8 Approximately 30% of all CT chest exams have incidental lung nodules.8 These nodules can even be noted on scans intended to image other parts of the body, like the abdomen or spine, but which capture part of the lungs. Although the majority of incidental lung nodules detected represent benign disease, the risk that a nodule represents lung cancer increases with increasing size of the nodule, radiologic characteristics, and patient risk factors.9 Evaluation or follow-up is determined based on the pretest probability that a lung nodule represents malignancy.
The Fleishner Society established guidelines for management of incidental lung nodules categorized by nodule size. Small, low-risk nodules can often be followed with serial CT imaging, whereas larger, intermediate-, or high-risk nodules can require more advanced imaging and invasive tissue biopsy procedures. The approach to biopsy can vary by patient, entailing bronchoscopy-guided biopsy, CT, ultrasound guided-biopsy, or, in some cases, more invasive surgical biopsy. Evaluation and management of intermediate- or high-risk nodules is best performed by pulmonary subspecialists.
Challenges With Incidental Lung Nodule Management
Only 36% of incidental lung nodules receive appropriate workup or follow-up.10 Substandard follow-up care is associated with known structural inequities and health disparities. Some challenges include the shortcomings in the methods of reporting or communicating incidental findings results to patients and appropriate providers as detailed above. Additional barriers are seen when those managing incidental pulmonary nodules are unaware of evidence-based guide-lines or lack access to the subspecialty expertise to further evaluate the lung nodule.
Most large institutions have a lung nodule program or clinic dedicated to the evaluation and management of both lung cancer screening and incidental lung nodules. While these nodule programs usually include a pulmonologist, highly effective programs include multidisciplinary specialties such as thoracic surgery, interventional radiology, chest radiology, radiation oncology, pathology, and medical oncology. Despite having a well-equipped multidisciplinary team, these lung nodule programs often rely on a passive referral process, which can miss numerous patients with intermediate- or high-risk lung nodules. Even patients evaluated in lung nodule programs or clinics can be lost to follow-up without effective tracking.
Nurse Navigator Challenges
In a lung nodule program, the nurse navigator plays a pivotal role in facilitating timely access to care, coordinating and expediting diagnostic testing, addressing patient barriers to care, ensuring punctual adherence to follow-up, and communicating and educating patients and referring providers.11
One of a nurse navigator’s many roles includes keeping track of patients with lung nodules to ensure they receive follow-up, whether that be a procedure, close interval imaging, or long-term follow-up in 1 to 2 years. For many, this process involves manually updating outdated Excel spreadsheets, which can be time consuming and unreliable. Software programs can help nurse navigators track patients, but they still require significant data entry while manually and separately referencing the patient’s electronic health record (EHR). Transposition of this information can result in expected human error.
Additional steps are undertaken to set up reminders for nurse navigators to check if patients have undergone their next expected follow-up step. If patients are overdue for their follow-up, reminder messages sent by the nurse navigator via either electronic, phone, or letter communication can also be labor intensive.
Additionally, only patients referred to the lung nodule program undergo tracking by the nurse navigator, excluding a large proportion of patients within the health care system who are not being seen within the lung nodule clinic. This process relies on passive referral to the nodule program rather than proactive measures to ensure all patients get appropriate follow-up. Finally, lung nodule nurse navigators often maintain a separate tracking system for lung cancer screening.
Path to a Solution
At UCHealth, we became aware that numerous patients with incidental lung nodules were not getting appropriate follow-up. A few patients diagnosed with late-stage lung cancer were found to have had overlooked incidental lung nodules on a past imaging scan—a devastating missed opportunity for early detection and diagnosis. Like many others, our health system lacked standardized protocols and integrated systems to prevent patients like this from falling through the cracks.
In response, UCHealth created a taskforce to address these issues called the Haystack Committee, a reference that finding these lung nodules is like finding a needle in a haystack. The Haystack Committee was a multispecialty group comprised of members from multiple UCHealth sites including quality leaders, IT, and clinicians in pulm-onology, thoracic surgery radiology, and primary care. The commit-tee’s goal was to find a solution that created a safety net for all patients with incidental lung nodules. More, any solution should:
- Integrate seamlessly with UCHealth’s EHR
- Have the ability to identify and track a large number of patients
- Ensure standardized, evidence-based follow-up for all patients that was scalable, automated, and efficient in a large health care system
- Not result in drastic changes to workflow.
Additionally, if successful, the solution could be applied to incidental findings in disease states beyond the lung.
The Haystack Committee vetted multiple solutions and, in the end, chose the platform that best met the needs of our large and heterogenous health care system.
The Eon Solution
Eon offers an artificial intelligence (AI) solution that uses computational linguistics, specifically, natural language processing, to evaluate radiology interpretations to identify incidental lung nodules and their characteristics and store them in a database. It extracts pertinent information from radiology reports without changing radiology workflow with 98% precision. Patients within the database can then be stratified and triaged based on risk. Low-risk patients will be triaged to automated evidence-based follow-up, but high-risk patients are triaged to provider review. The AI platform is integrated with the EHR to automatically send tailored communication to patients to inform them of the incidental finding. The platform then tracks any follow-up imaging and exams and updates the database when these tasks are performed for ongoing surveillance or completion of additional next steps. If patients are overdue, the platform sends automated reminders to both patients and providers to ensure timely and appropriate follow-up. Real-time analytics can be performed to evaluate various metrics and identify program deficiencies to further develop future solutions.
CU Innovations, a branch of the University of Colorado that specializes in developing ventures and partnering with commercial technology, partnered with Eon on this solution. Through this part-nership, we were able to develop a universal standard operating process that was applicable to multiple UCHealth sites with varying resources. The process integrated evidence-based guidelines with specialized clinical expertise to create a unique clinical pathway for patients identified with incidental lung nodules. Input from primary care was considered early in the planning process to ensure that the frequency and content of communications with patients and providers was appropriate to minimize distress and inbox fatigue. This standard operating process has since been reviewed and revised based on feedback from patients and providers.
The pathway automatically set recommended follow-up based on the Fleischner Society criteria for nodules < 8mm in size.12 Given the higher risk to represent lung cancer and the additional complexity in management and need for subspecialist evaluation, our recommendation for people with nodules > 8mm was referral to our lung nodule clinic.
Volumes and Adherence
The incidental lung nodule program went live in September 2022 in UCHealth’s North and Metro regions. Data analytics were used to report out performance. Almost immediately both regions were seeing tremendous volumes of new and follow-up exam tracking. Each month there were over 1000 new patients identified within the Eon system and between 300 and 600-plus follow-up exams tracked. By the fourth quarter, the percentage of actively managed patients within the lung nodule program increased 2514% to a total of 4349 (Figure 1). Patients’ return rates increased by 54% to 90% and on-time return rates increased by 155% to 82% (Figure 2).


Due to the significant volumes of new patients identified, our nurse navigators shared that additional help was needed. While most new patients identified had lung nodules < 8mm, more than one-third (35.7%) had nodules > 8mm that required referral to the lung nodule clinic and nurse navigator coordination of care. Therefore, UCHealth again enlisted help from Eon through its Care Management Team of nurse navigators. Trained in lung nodule management and familiar with UCHealth’s clinical pathway, Eon’s nurse navigators review patient data and radiology reports to verify next follow-up and facilitate communication with patients and providers. While the UCHealth nurse navigators continued to manage the > 8mm, high-risk patients and facilitate their referral to the nodule clinic, patients with lower-risk nodules (< 8mm) were managed by Eon’s Care Management Team. With this change, we were able to reduce the average time until next step was recommended from 34 days to 5 days from the exam.
Program Outcomes
By the beginning of Q4 2022, over 38000 imaging exams were analyzed by the Eon software. More than 6500 patients were added into active surveillance for incidental lung nodules. Most importantly, 274 lung cancers were diagnosed. Of the 274 lung cancers diagnosed, 92% were non–small cell lung cancer (NSCLC) and 8% were small cell lung cancer. Of the NSCLCs, 70% were lung adenocarcinoma and 20% squamous cell carcinoma.
Remarkably, 40% of the patients newly diagnosed with lung cancer within our program had stage I disease (Figure 3). This is significantly higher than the national average of about 20% of new lung cancer diagnosed at stage I.13
Cost-Effectiveness
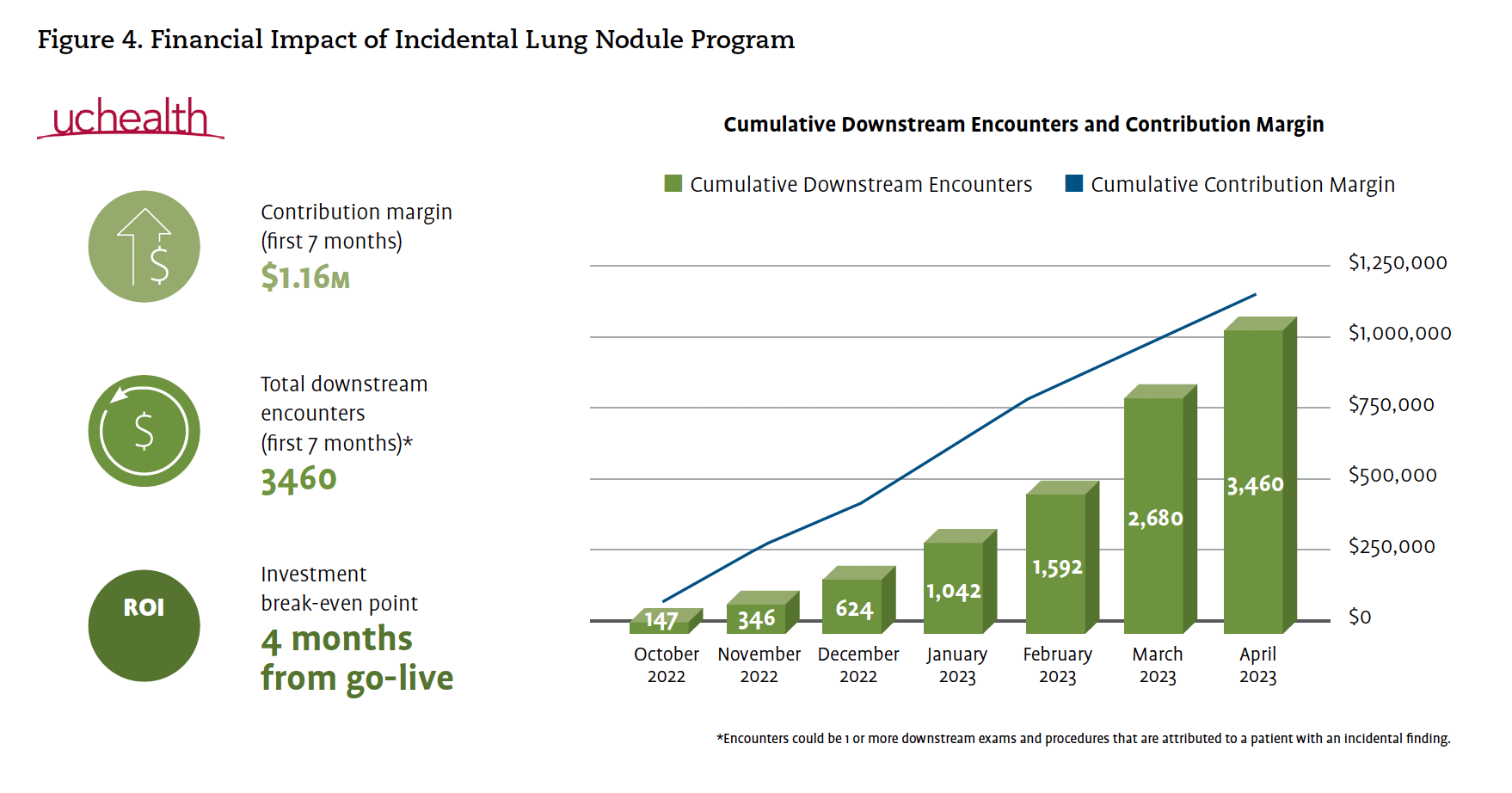
In addition to demonstrating the incidental lung nodule program’s clinical benefit to our patients, we were also able to show that investment in this AI platform was cost-effective. Within the first 7 months, the contribution margin to the health care system was $1.7 million. The program led to 3460 downstream encounters at 7 months and over 5000 downstream encounters at 18 months. We were able to achieve a return on investment within 4 months (Figure 4).
Collateral Benefit to Lung Cancer Screening
Lung cancer screening is also built into the AI software. The platform separates patients undergoing lung cancer screening with yearly low-dose CT into a different cohort. Next recommended follow-up is set based on Lung-RADS criteria, evidence-based guidelines designed specifically for lung cancer screening. Similarly, patients receive tailored letters with their result and follow-up recommendations, as well as automated reminders if they are overdue for their next exam.
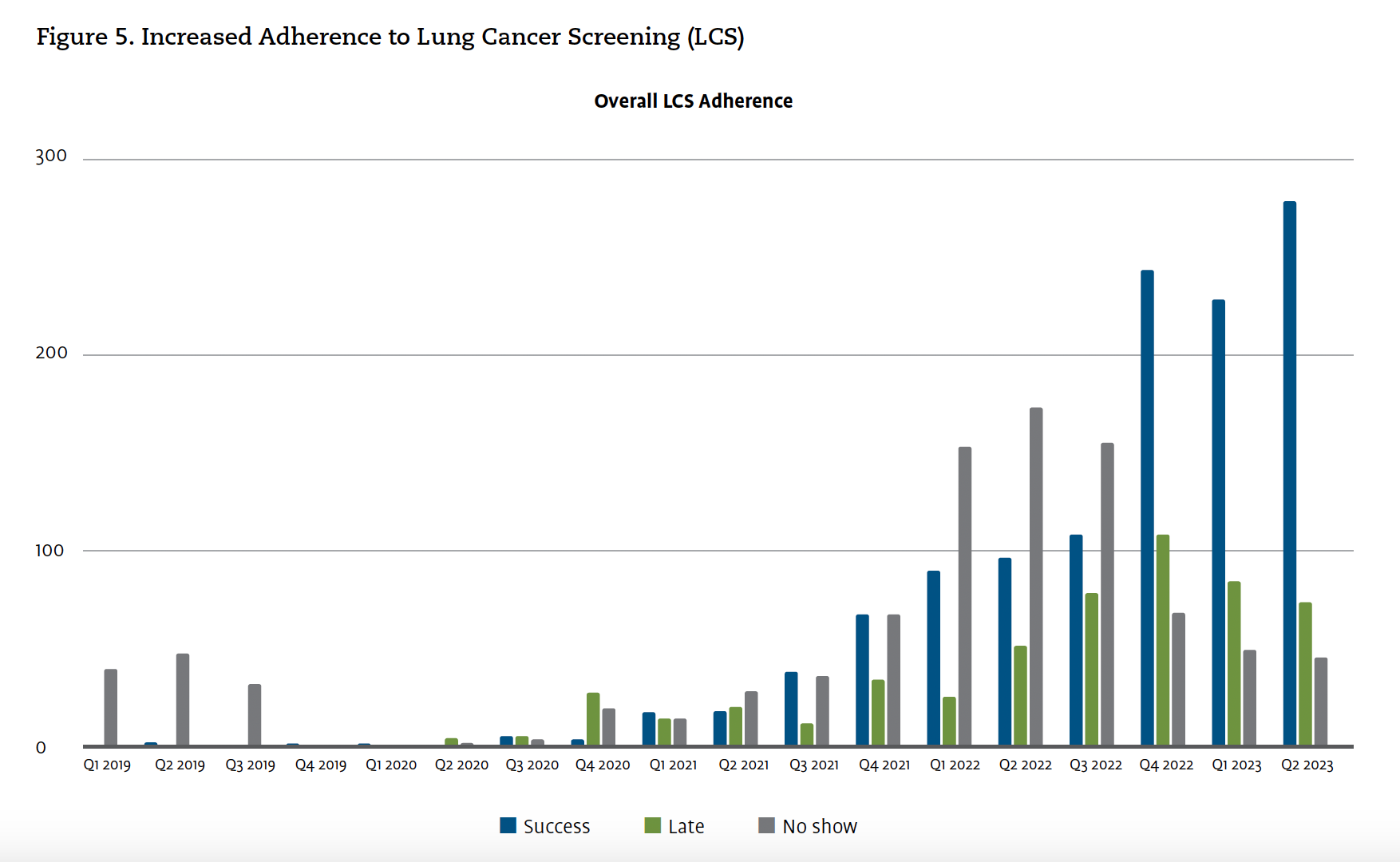
At 1 year, over 2300 patients were added to lung cancer screening and overall lung cancer adherence rates increased significantly (Figure 5). We believe that with this AI solution, adherence rates for yearly lung cancer screening will continue to increase each year.




Nurse Navigator Perspective
At 1 year, our nurse navigators reflected on the incidental lung nodule program. They acknowledged the novel ability of the AI platform to identify nearly all incidental lung nodules throughout our large health system. The fear of missing a patient within our system with a worrisome lung nodule has started to dissipate. Unlike the previous labor and time-intensive systems, this platform allowed nurse navigators to focus on high-risk patients by automating letters and reminders and offering additional assistance from the Eon Care Management Team. More, nurse navigator time and efforts were focused on 1 universal platform to manage both incidental lung nodule patients and lung cancer screening patients. Overall, nurse navigators noted improved efficiency and reporting for both cohorts.
Future Directions
We have subsequently expanded the lung nodule tracking program to additional UCHealth sites. In partnership with Eon, we also hope to build a tracking module for patients for surveillance after patients have been successfully treated for lung cancer.
With the success of the incidental lung nodule and lung cancer screening platform, UCHealth plans to expand our incidental tracking program to other disease states, including pancreas lesions and thyroid nodules. This expansion creates an additional safety net for patients with incidental findings of pancreatic cysts or masses and thyroid nodules to ensure necessary and appropriate follow-up.
Nina A. Thomas, MD, is assistant professor of medicine and director of the Thoracic Malignancy Pillar of Center for Lung and Breathing, Division of Pulmonary Sciences & Critical Care Medicine, University of Colorado School of Medicine in Denver, Colorado. Stephanie Brown, RN, is a nurse navigator at UCHealth in Aurora, Colorado. Lindsay Miller, PMP, is manager, Innovation & System Project Management, UCHealth in Denver, Colorado.
References
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin.2024;74(1):12-49. doi:10.3322/caac.21820
- Kratzer TB, Bandi P, Freedman ND, et al. Lung cancer statistics, 2023.
Cancer. 2024;130(8):1330-1348. doi:10.1002/cncr.35128 - National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;258(1):243-253. doi:10.1148/radiol.10091808
- Fedewa SA, Kazerooni EA, Studts JL, et al. State variation in low-dose computed tomography scanning for lung cancer screening in the United States. J Natl Cancer Inst. 2021;113(8):1044-1052. doi:10.1093/jnci/djaa170
- Lumbreras B, Donat L, Hernandez-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol. 2010;83(988):276-
289. doi:10.1259/bjr/98067945 - Hansra SS, Loehfelm TW, Wilson M, Corwin MT. Factors affecting adherence to recommendations for additional imaging of incidental findings in radiology reports. J Am Coll Radiol. 2021;18(2):233-239. doi:10.1016/j.jacr.2020.02.021
- Mortani Barbosa EJ, Jr., Osuntokun O. Incidental findings in thoracic CTs performed in trauma patients: an underestimated problem. Eur Radiol. 2019;29(12):6772-6779. doi:10.1007/s00330-019-06313-6
- Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015;192(10):1208-1214. doi:10.1164/rccm.201505-0990OC
- Mazzone PJ, Lam L. Evaluating the patient with a pulmonary nodule: a review. JAMA. 2022;327(3):264-273. doi:10.1001/jama.2021.24287
- Pyenson BS, Bazell CM, Bellanich MJ, Caplen MA, Zulueta JJ. No apparent workup for most new indeterminate pulmonary nodules in US commercially-insured patients. J Health Econ Outcomes Res. 2019;6(3):118-
129. doi:10.36469/9674 - Doerfler-Evans RE. Shifting paradigms continued-the emergence and the role of nurse navigator. J Thorac Dis. 2016;8(Suppl 6):S498-500. doi:10.21037/jtd.2016.04.03
- MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: From the Fleischner Society 2017. Radiology. 2017;284(1):228-243. doi:10.1148/radiol.2017161659
- SEER Cancer Stat Facts: Lung and Bronchus Cancer. National Cancer Institute. Accessed February 6, 2025. https://seer.cancer.gov/statfacts/html/lungb.html















